UnitedHealth Group Q4 and 2024 Full Year Earnings
Between Cyberattacks and Death of UHC CEO, 2024 Was A Challenging Year for UNH
UnitedHealth Group (UNH) kicked off the "Big Six Payor" earnings season, setting the stage for reports from Cigna, CVS, Humana, Centene, and Elevance over the next six weeks. On Thursday, UNH reported its Q4 and full-year 2024 earnings before the market opened. While the stock initially dropped 5% in pre-market trading, it ended the day down 3.5%. The market reacted negatively to an elevated Medical Care Ratio (MCR), which missed estimates by 150 basis points. Below, I’ll outline the five key factors contributing to this miss.
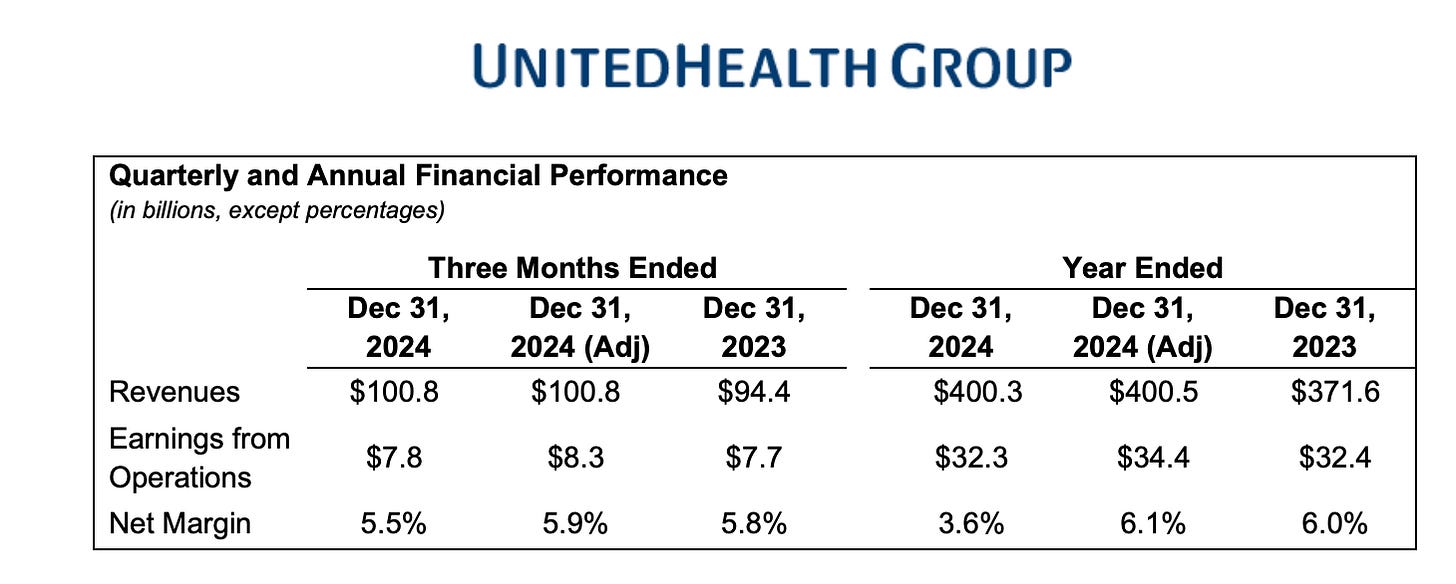
Despite the market's response, UNH posted strong revenue growth, rising from $371.6 billion in 2023 to $400.3 billion in 2024. Earnings per share (EPS) also climbed to $27.66, representing an 8.1% increase.
Andrew Witty, UNH's CEO, opened the call by addressing systemic challenges in healthcare, paying tribute to former UHC CEO Brian Thompson, and discussing OptumRx's value proposition amid the FTC’s ongoing scrutiny of PBMs. He also touched on the rising costs of GLP-1 drugs and the pricing disparity between the U.S. and Europe. Witty announced OptumRx's plan to phase out rebate-based incentive models by 2028, a topic I’ll address further below.
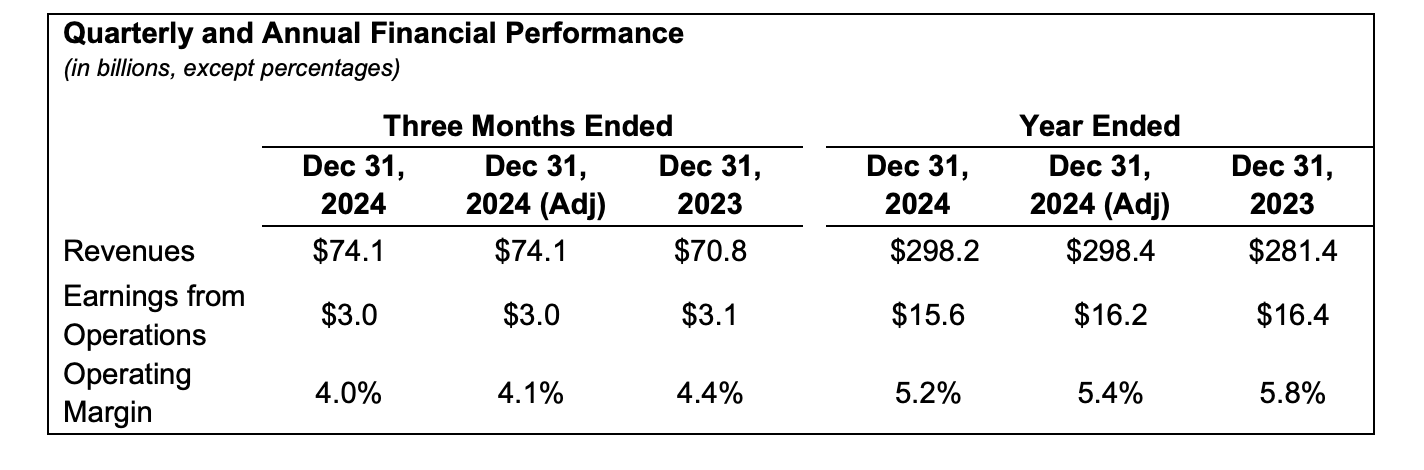
UnitedHealthcare (UHC)
Revenue & Membership
UHC’s revenue grew nearly 6% year-over-year, driven by membership growth of 2.4 million lives.
Medicare Advantage
UHC currently serves 9.4 million Medicare Advantage (MA) beneficiaries and expects to add 800,000 members in 2025. Witty highlighted the opportunity in converting the 50% of Americans still on traditional Medicare to MA plans, with UHC targeting annual growth of 7%-9%. They cited a successful open enrollment period, adding 400,000 new members—quadruple last year's figure. UHC also achieved a well-balanced mix of members across SNP, dual-eligible, and traditional MA segments, which has been a challenge in prior years.
Medicaid
UNH ended 2024 with 7.4 million Medicaid members and sees continued growth opportunities as redeterminations taper off. Their recent win in Georgia and expanded partnerships in Michigan, Idaho, and Nevada underscore their Medicaid strategy. Some MCR headwinds stemmed from Medicaid, but the company emphasized strong state partnerships and improving reimbursement alignment. UNH expects acuity misalignments from 2024 to subside moving forward.
Elevated Medical Care Ratio (MCR): Key Drivers
CFO John Rex broke down the elevated 2024 MCR into two categories with 5 separate causes:
Primary Factors (70% of the Impact):
1. Consumer Mix: Lower-than-expected Medicare Advantage growth due to competitive plan designs for 2024.
2. Medicaid Timing Mismatch: Misaligned health status of Medicaid members and state rate updates.
Keep reading with a 7-day free trial
Subscribe to The Healthcare Economy to keep reading this post and get 7 days of free access to the full post archives.