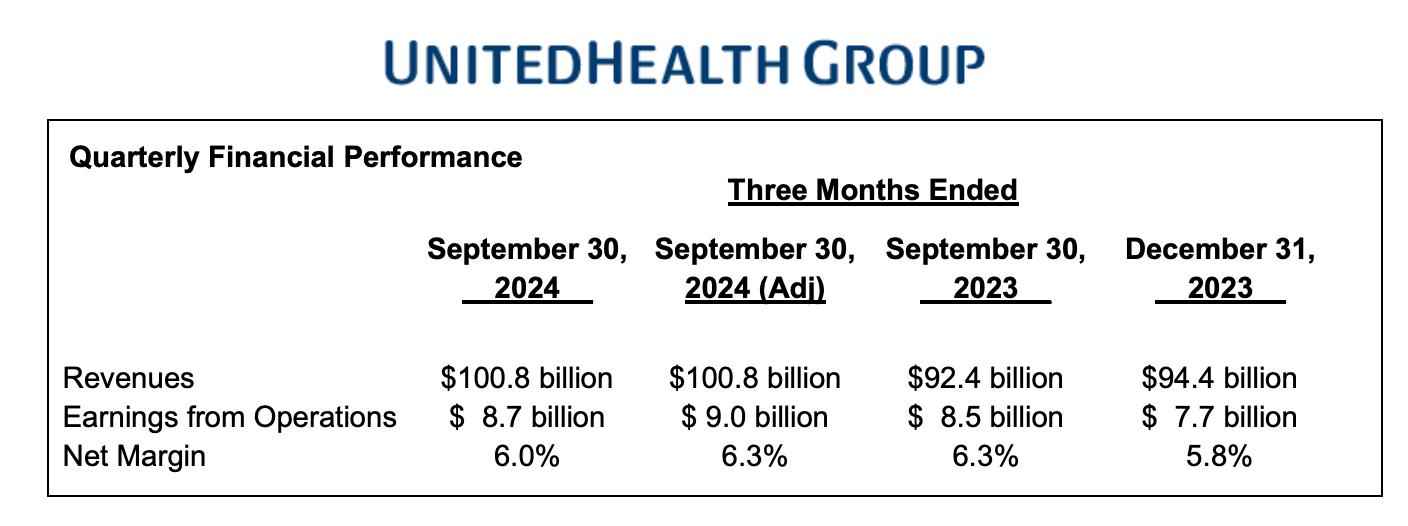
UnitedHealth (UNH) kicked off the “Big Six Payors” earnings period last Tuesday with their Q3 earnings call. Overall, it was pretty solid, despite the initial reaction from Wall Street (a 10% drop). UNH wrapped up Q3 with $100.8 billion in revenue, which is $8.5 billion more than Q3 2023, showing good growth for a company of this size (9% QoQ).
The main concern from the market seemed to be the elevated spending on the care side, something that’s been a challenge for all payors over the past few quarters. UNH pointed out that there’s been a lag in state Medicaid reimbursements (due to higher acuity, higher coding intensity from hospitals), and they also flagged a new concern: increased high-cost drug utilization. This is being driven by the IRA’s elimination of coinsurance during the catastrophic phase (the second half of the year). UNH admitted they were caught a bit flat-footed by the unexpected rise in drug costs, as they hadn’t fully anticipated drug manufacturers' ability to drive usage.
In general, though, this was a strong call for UNH, especially with their emphasis on Value-Based Care across their business units. They stressed that OptumHealth is adding more lives in value-based arrangements (4.7 million members). Below are my key takeaways and thoughts on what this could mean for the broader healthcare space.
AI and Gold Card
UNH launched the first national gold card program, which will cut down on prior authorizations by 500,000 annually for qualified in-network providers. The gold card initiative will be great for providers, patient and even UNH as they look to reduce internal costs. They also talked about some generative AI workflows they’ve developed for nurses, which are driving higher NPS scores since nurses now have more time to spend with patients/members. On the technology front, UNH also highlighted how AI is helping them build tech solutions faster and more efficiently.
Medicaid
Most of the big Medicaid payors had expected states to increase PMPM (per member per month) reimbursements in the second half of the year, but according to UNH’s earnings call, that doesn’t seem to be happening. I’ve mentioned this before, but the risk pool has shifted: many of the beneficiaries added to Medicaid post-COVID were healthier, but now that those healthier members have been removed (through redeterminations), the current population is more complex and expensive to manage. As a result, payors like Centene, Elevance, CVS, Molina, and UNH are dealing with a PMPM that’s lower than the cost to provide care to these riskier patients However, UNH was excited about some recent Medicaid contract wins in Massachusetts, Colorado, Rhode Island, Florida, and Michigan. Additionally, they were really excited about some of the behavioral health partnerships they are seeing in their Medicaid business to augment some of their RFP efforts.
Medicare Advantage
Medicare Advantage continues to face challenges from elevated utilization, the impact of the IRA, and ongoing CMS rate cuts. Despite these headwinds, UNH remains confident that Medicare Advantage still offers significantly more value than traditional Medicare. They believe their CMS Star ratings were strong year-over-year and that they’ll continue to lean into the space by leveraging assets like OptumRx, OptumHealth, and OptumInsight to provide more value to beneficiaries. Across all lines of business, UNH added 2.4 million members in 2024 and plans to continue growing through open enrollment.
Commercial Book of Business
UNH feels like they had a strong selling season in their commercial book of business and plan to focus more on partnerships with hospitals. They also see OptumRx as a key player in driving down drug costs and helping employers manage behavioral health offerings more effectively in 2025.
Elevated RX Costs in Medicare
There was some anticipation of changes from the IRA in Medicare Advantage and
Keep reading with a 7-day free trial
Subscribe to The Healthcare Economy to keep reading this post and get 7 days of free access to the full post archives.