Humana hosted their investor day in Louisville on Monday (6/16) to give a review of where they sit in 2025 and where they are headed over the next several years to drive shareholder value in the Medicare Advantage space. This was a vital investor day as some of the investor calls have been light on content, as Jim Rechtin has made the opening remarks very brief and quickly moved into the Q&A section of the call. With this format, many in the investment community were anticipating getting a bit more granular on the current state, the path forward in MAPD, and what the timeline is for recovery. Below are the main takeaways which I found to be interesting given some of the historical storylines.
Critical Discussion of the Past 10 Years of Strategy
Jim Rechtin was consistent and was able to cover his usual guiding pillars, which he has consistently talked about since assuming the CEO role last summer. These drivers are at the core of how he sees Humana generating value across its business:
Clinical Excellence — The primary driver of Humana’s medical expense ratio. By delivering high-quality care and improving outcomes, the company aims to manage costs and enhance value-based performance.
Operating Leverage / Administrative Efficiency — This driver underpins Humana’s admin expense ratio. Rechtin’s strategy calls for disciplined management of overhead, leveraging automation and scale to improve margins.
Product and Experience — The key engine of member growth. Humana is focused on designing competitive products and delivering superior member experiences to attract and retain beneficiaries.
Disciplined Capital Deployment — Humana’s approach to balancing organic growth, strategic acquisitions, and returning capital to shareholders. This ensures investments align with long-term strategy while preserving financial strength.
Along with this reiteration, what surprised me was he was a bit more vocal on the historical strategy of the organization being highly focused on driving STAR ratings. In his opinion, he believed that the organization was primarily focused on driving for a metric which they had little control over as CMS continues to shift how it evaluates or accounts for it. He referenced that the STAR rating collapse from October came as a wake-up call for them to begin to drive the four pillars to take their destiny into their own hands. They believe Humana’s path to steady, profitable membership growth hinges on controlling what’s within its power: driving better clinical outcomes and lower medical costs through aligned provider incentives, tools that are actively used, and strong influence over how its network operates. Jim Rechtin noted that this focus, combined with tight control over operating leverage, marks a shift from how Humana historically approached growth. In past years, Humana often faced a disadvantage in MACVAT (Medicare Advantage Comparative Value Assessment Tool) scores, a benchmark that evaluates the overall value of a plan’s benefits relative to competitors, because its benefits tended to lag behind rivals. This gap may have been partly due to Humana having fewer or less mature value-based agreements than some peers, limiting their ability to translate clinical cost savings into richer benefits. Despite this, Humana kept pace with the market by delivering industry-leading customer service and leveraging a superior distribution network. Now, they aim to reduce reliance on just service and their sales network to overcome benefit gaps and instead grow by improving the core drivers of cost, quality, and efficiency that it can directly control. In the current state of Humana, he believed that the service portion allowed them to be poor operationally, poor with retention, and poor with overall engagement with the members over multiple years.
Sponsored by Dave Breininger at Talent Wave
Talent Wave connects exceptional individuals with visionary healthcare companies through a personalized, innovative approach. . Learn more at www.talentwaveassociates.com. Contact David at (567) 304-3102 or DBreininger@talentwaveassociates.com
Longer Relationships
V28 is becoming a huge headwind for health plans that are focusing on the Medicare Advantage space, which is changing the way these plans acquire and try to build profitable longer-term relationships with members. In the past, the previous V21/V22 risk adjustment systems used the ICD-9 coding for ailments, which allowed for more stacking of codes for health plans to get higher reimbursement. Under the V28, it has been scaling in over the past 3 years with 2025 being fully to the new model, which uses ICD-10 coding and does not allow stacking of codes so it better represents comorbidities to more accurately reflect treatment for patients. In this new model, Humana wants to focus on driving longer-term relationships with their customers so that they can control engagement with the members. When they have them over multiple years, they can drive meaningfully better outcomes through consistent care instead of some of the fragmentation that they believe exists from members jumping from plan to plan. They have been meeting with the members and getting feedback that the system is too complex to navigate, the member needs help guiding them, and telling them what they need to do at every step. Jim Rechtin believes that Humana has the data and technology to make this happen in the near term to be able to drive a meaningful impact on the business and care. He feels that the organization was wholly focused on one lever, and with this new strategy to align with the member along with focusing on multiple levers, it can drive a better MAPD plan.
George Renaudin (President Humana/Insurance Segment)
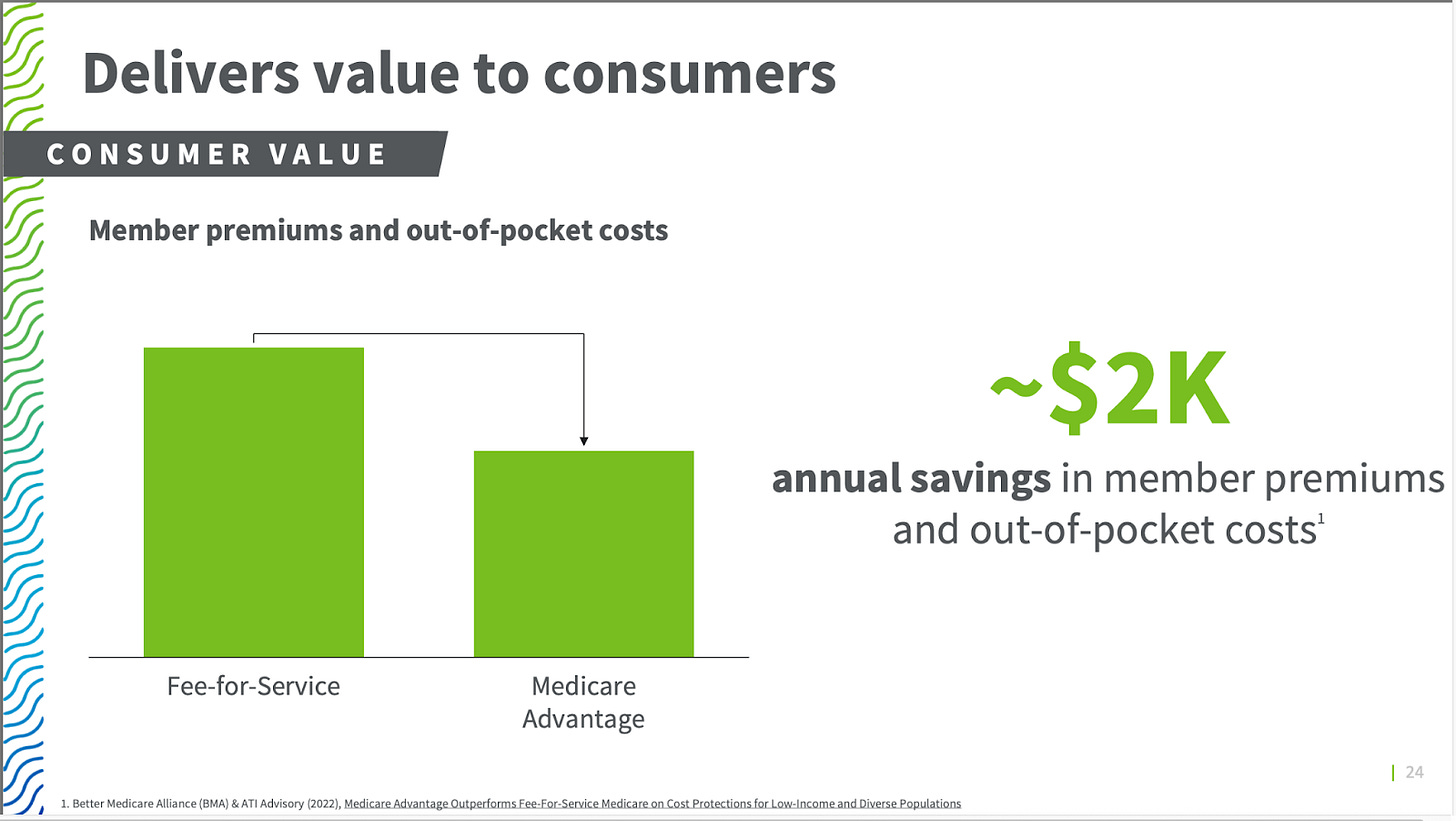
George Renaudin stepped in to cover why they still see the Medicare Advantage business as an attractive business as they look to recover over the next 3-4 years. He highlighted that MA is fundamentally attractive because it delivers superior health outcomes, reduces costs for beneficiaries, enjoys robust bipartisan political support, demonstrates consistent enrollment growth, and offers an appealing long-term margin profile of 3% or higher for Humana. Renaudin emphasized that MA outperforms traditional fee-for-service Medicare across nearly every measure of quality, with members receiving more preventive care, such as critical screenings and wellness visits, which translates to better outcomes and lower costs. He noted that MA members consistently see thousands of dollars in annual out-of-pocket savings and gain access to supplemental benefits that original Medicare doesn’t offer, such as dental, vision, hearing, transportation, and fitness programs—features that drive satisfaction and retention. In fact, once seniors enroll in MA, they rarely switch back to fee-for-service Medicare. Renaudin also stressed that MA delivers taxpayer value by improving care efficiency, reducing unnecessary hospitalizations, and lowering readmission rates. This, combined with the growing senior population and increasing MA penetration, creates a natural enrollment tailwind for Humana. Political support for MA is deeply rooted in its popularity among constituents, with many congressional districts seeing over 60% of Medicare beneficiaries enrolled in MA. Despite cyclical pressures on margins, Humana has repeatedly shown it can adapt, whether during the Affordable Care Act or the COVID pandemic, by improving quality, managing costs, and stabilizing profitability. With 20% of MA members nationwide carrying a Humana card and leadership positions in key markets, Renaudin expressed confidence that Humana is well-positioned to capitalize on these trends and deliver sustained shareholder value.
COO Comments (Lisa Stephens)
COO Lisa Stephens outlined Humana’s clinical excellence strategy, emphasizing a cohesive approach built around three core levers: achieving a complete understanding of each member’s health, delivering care and experiences that improve outcomes and trust while closing Stars gaps, and implementing innovative clinical programs that lower total cost of care while increasing accessibility, personalization, and effectiveness. At the heart of this strategy is a commitment to “doing the right thing for our members.” Stephens highlighted five enabling capabilities that bring this vision to life: industry-leading interoperability (with over 60% of providers already connected and a goal of surpassing 80%), point-of-care alerts that embed insights into providers’ workflows, aligned incentives that focus everyone on better health, deeper member engagement at every touchpoint, and robust use of data and analytics to drive smarter, faster decisions. The intended result is a win for members, the company, and shareholders alike.
Stephens offered examples of how this strategy is being operationalized, with a particular focus on moving upstream through proactive, preventive care. As Jim Rechtin covered in his opening remarks, annual wellness visits are a key starting point, enabling accurate diagnoses, closing Stars gaps, and setting the stage for innovative care delivery. Humana is driving more members to these visits through new tactics, including partnerships with CenterWell Primary Care and embedding clinical insights directly into providers’ systems. This comprehensive view of member health allows Humana to improve quality, enhance Stars performance, and reduce avoidable hospitalizations. Given that CMS adjusts the Stars thresholds annually, effectively grading on a curve, Stephens stressed that continuous improvement is essential. Every gap closed means better screening rates, stronger chronic disease management, and healthier members, all of which are core to Humana’s long-term growth and margin stability.
Diabetes/Chronic Disease and Pharmacy
One of the areas that Lisa Stephens discussed was their commitment to have the pharmacy team get more connected with patients as the weighting for medication adherence is tripling. One of the new things she mentioned was the pharmacy reaching out to schedule an appointment with patients post-discharge to do an MTM and begin to build a relationship. They are really working to get the pharmacy team engaged in driving down A1C for diabetes chronic patients, as this is another highly weighted measure for the STAR ratings as it causes vision and kidney complications. Beginning to connect with over 90,000 members a month to schedule wellness visits and close gaps in care with the longer-term goal of driving the member to be more engaged in their care. They are also going to be using CenterWell in Home to drive some additional wellness visits in the home for chronic patients in conjunction with CenterWell Pharmacy delivery.
Medicaid
Keep reading with a 7-day free trial
Subscribe to The Healthcare Economy to keep reading this post and get 7 days of free access to the full post archives.