Elevance Q1 of 2025
Tariff and General Market Sluggishness Steals The Thunder For Elevance in Q1
Sponsored by Dave Breininger at Talent Wave
Talent Wave is transforming how healthcare organizations discover and retain top-tier talent. Led by industry specialist David Breininger, Talent Wave connects exceptional individuals with visionary healthcare companies through a personalized, innovative approach. . Learn more at www.talentwaveassociates.com. Contact David at (567) 304-3102 or DBreininger@talentwaveassociates.com
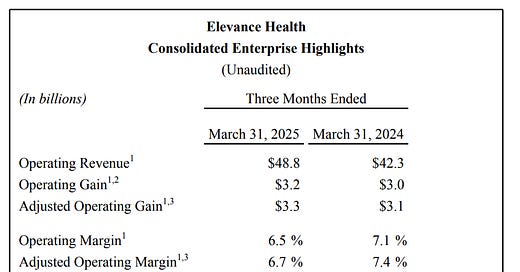
Elevance was the second of the “Big Six Payors” to report earnings Tuesday morning before the bell, delivering a beat on both top line and EPS. The stock is up over 3% since then, although the reaction was a bit muted compared to what I expected given the strength of the quarter. Revenue grew 15% quarter over quarter, driven by Medicare, ACA/Marketplace growth, and acquisitions within the Carelon business. While operating margin fell 60 basis points due to slightly higher Medicaid costs, they continue to drive towards greater efficiency to offset higher utilization. Overall, it was a strong call and they continue to make progress toward their vision of growing Carelon and investing in accretive areas to manage members more efficiently. After reading through the earnings transcript, these were the highlights for me:
Health Insurance Business
They grew membership by 99,000 since the beginning of the year, reaching 45.8 million members. They also posted better-than-expected retention in Medicare Advantage and strong growth in the ACA/Marketplace segment. Health Benefits revenue grew 10.8%, although operating margin fell 70 basis points.
Medicaid
They continue to make progress on rate alignment, with April adjustments coming in as expected and early discussions underway for the July cohort, which represents about 33% of their Medicaid business. Utilization is trending lower versus Q4, and they view the first half of the year as a stabilization period, with the back half benefiting from additional revenue from state partners. These conversations reflect a shared understanding with states about the need to align reimbursement with the current level of member acuity. Their long-term care model which integrates home-based services, behavioral health, and care coordination continues to deliver strong outcomes at lower cost, aligning with what we hear on UNH calls regarding OptumHealth. Overall, this was a good look at their membership growth both quarter over quarter and from the beginning of the year.
Medicare Advantage
Keep reading with a 7-day free trial
Subscribe to The Healthcare Economy to keep reading this post and get 7 days of free access to the full post archives.