Centene Reports Q4 Earnings and Full Year 2024
Centene Continues to execute on their strategic initiatives
Centene was the fourth of the “Big Six Payors” to report earnings before the market opened on Tuesday. Despite a strong performance and raising 2025 guidance by $4 billion, the market reacted negatively, with the stock finishing down 9% over the past four trading days. Revenue grew to over $163 billion for the year, a 6.5% increase over 2023, but investor concerns centered on rising medical expenses in Medicaid, Centene’s core business.
That said, after reviewing the earnings and financials more closely, I think Centene actually had a strong year. They effectively managed Medicaid’s post-COVID acuity misalignment, put Medicare STAR ratings back on a solid path, and continued to expand in the ACA/Marketplace.
Medicaid
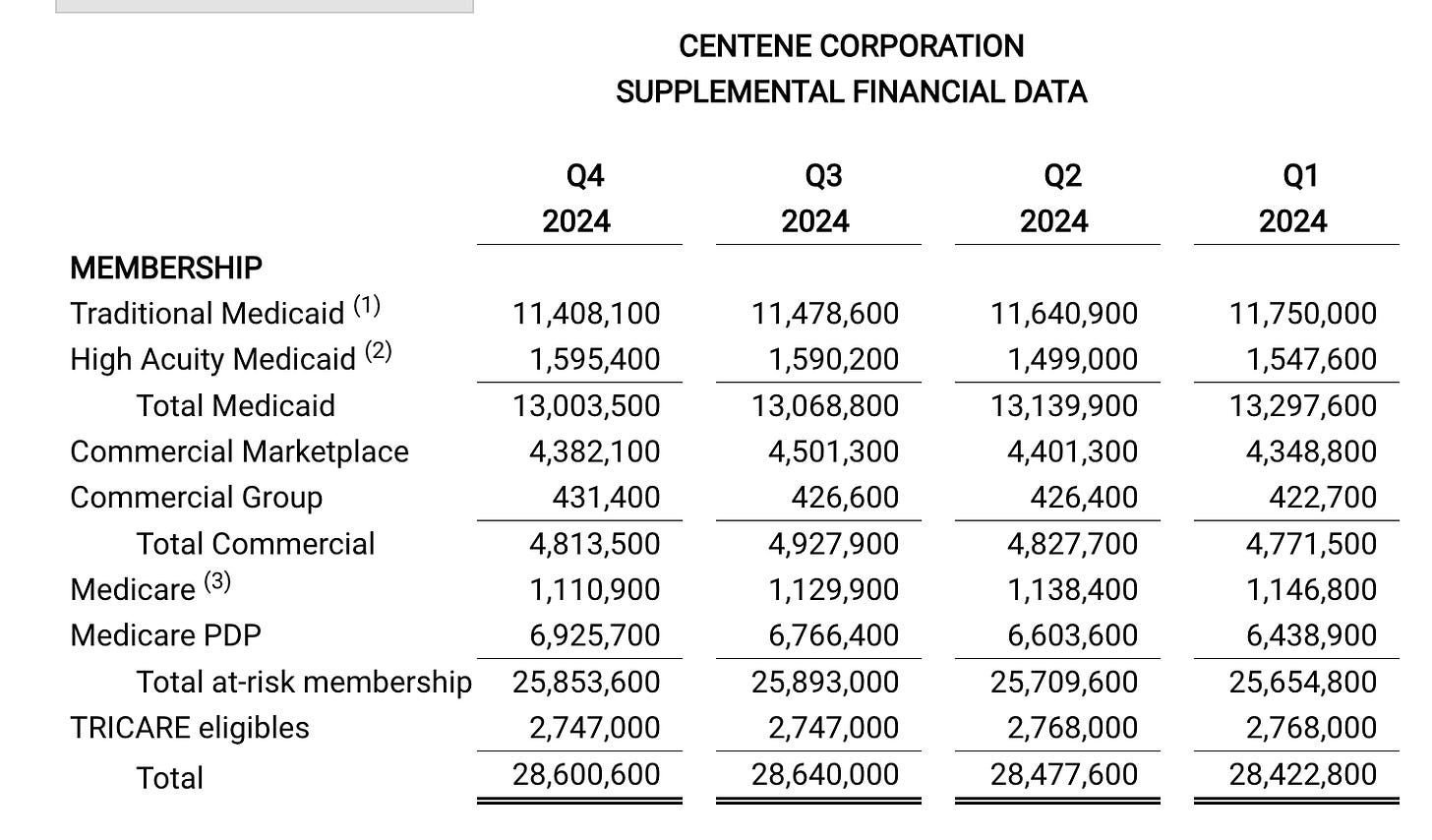
Centene is the largest Medicaid provider in the U.S., covering over 13 million members—down from 14.5 million post-redetermination. They view 2025 as a stabilization year, expecting to resume membership growth while aligning reimbursement rates with care costs.
For 2024, they set their medical benefits ratio (MBR) at 92.5%, leading to a 4.5% rate increase from 40% of their state partners (cohort starting 1/1/25). With Medicaid bid cycles returning to normal post-pandemic, Centene anticipates a more predictable operating environment. They also referenced ongoing litigation in Georgia and Texas but expressed confidence in securing key contract wins in 2025.
ACA/Marketplace (Ambetter)
Centene remains the largest player in the ACA/Marketplace, starting 2024 with over 5 million members. The overall market has doubled over the past five years to 24 million members, growing another 13% this year.
The big question is whether premium subsidies will be extended beyond 2024. Centene stated in their investor day and earnings call that without an extension, the ACA market could shrink by 20%-30%. Last year, they also saw some impact from new government rules requiring enrollees to file taxes to verify qualifying for lower-income subsidies. They anticipate some attrition in Q2 as members either fail to file taxes or no longer qualify for subsidies.
Notably, 75% of Centene’s ACA members are now enrolled in Silver-tier plans—an increase from around 70% in prior years. For more details on ACA metallic tier structures, refer to my previous Substack post.
ACA (ICHRA)
Centene is leaning into the Individual Coverage Health Reimbursement Arrangement (ICHRA) space, targeting employers looking for alternatives to traditional group insurance. Under a 2020 Trump administration rule, employers can allocate pre-tax dollars for employees to purchase ACA plans, with reimbursement at year-end.
Centene is pitching ICHRA as a way for businesses to manage healthcare costs while transferring risk. This also serves as a hedge in case premium subsidies aren’t extended, giving them another growth avenue in the ACA segment.
WellCare/Medicare
Keep reading with a 7-day free trial
Subscribe to The Healthcare Economy to keep reading this post and get 7 days of free access to the full post archives.